Download the Whitepaper
By Crystal Son, MPH – Healthcare Analytics Director at Civis Analytics
We recently conducted research to answer a question that’s incredibly important to data scientists at Civis:
Can we scientifically convince increasingly skeptical parents to vaccinate their children against potentially lethal diseases?
The short answer is that we can.
At Civis, we specialize in scientific survey and message research, which we’ve learned from a long history in politics. We recently conducted a robust online study1 to find out how we could persuade skeptical parents around vaccination against human papillomavirus (HPV) — a prevalent sexually transmitted virus that can cause terminal cancer in both men and women. Sadly, just 16% of children in the United States are fully HPV-vaccinated by age 13. Even by age 17, less than half of kids in the U.S. are fully vaccinated.
Here’s what we learned:
First, non-vaccinator parents are the group most concerned about vaccine safety.
This isn’t totally surprising, and we mostly understand what’s at play here—see the chart below.
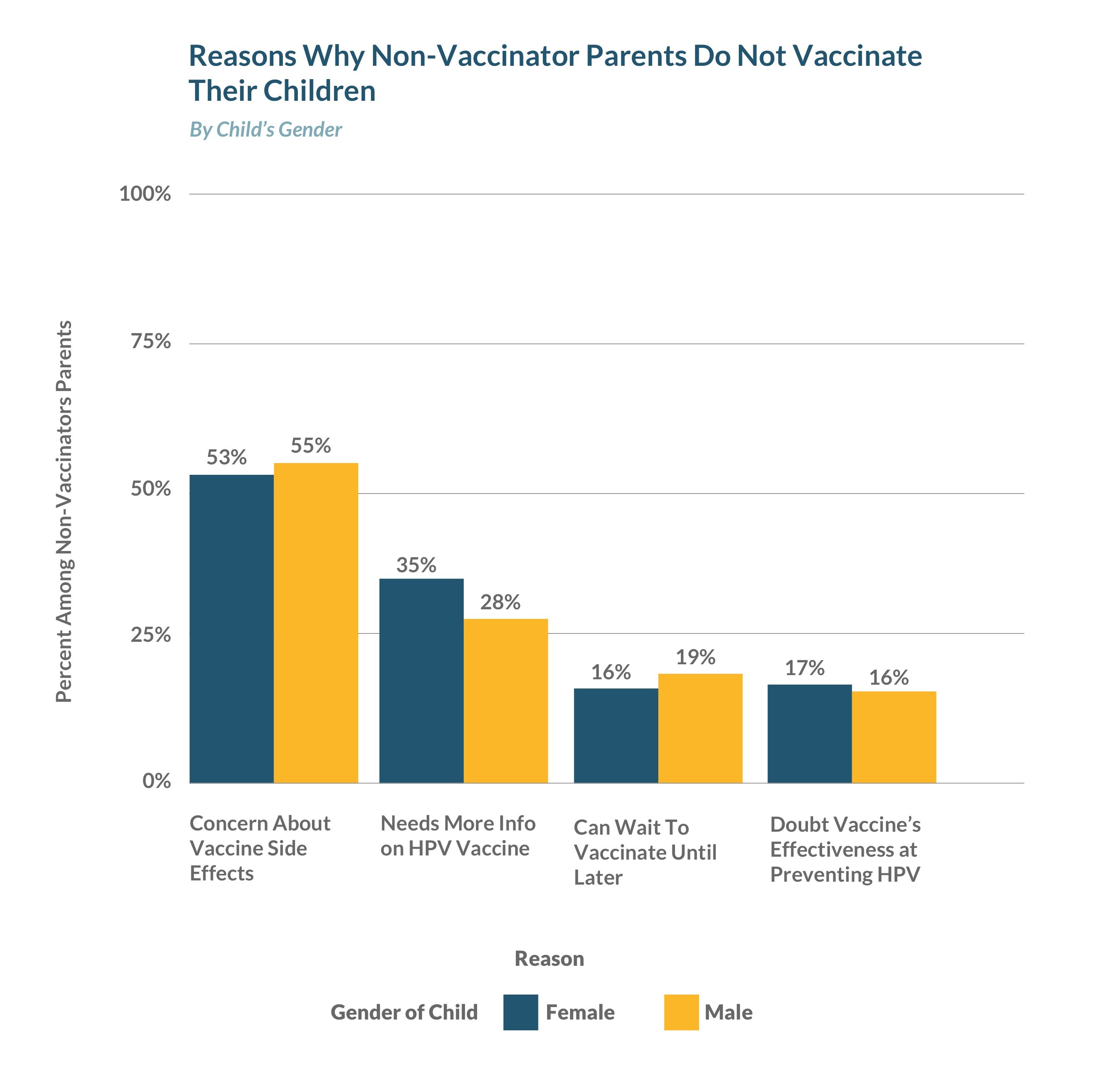
However, messages about vaccine safety are ineffective at persuading skeptical parents to vaccinate their kids. Instead, messages that focus on the consequences — specifically, linking HPV to Cancer — are far more effective.
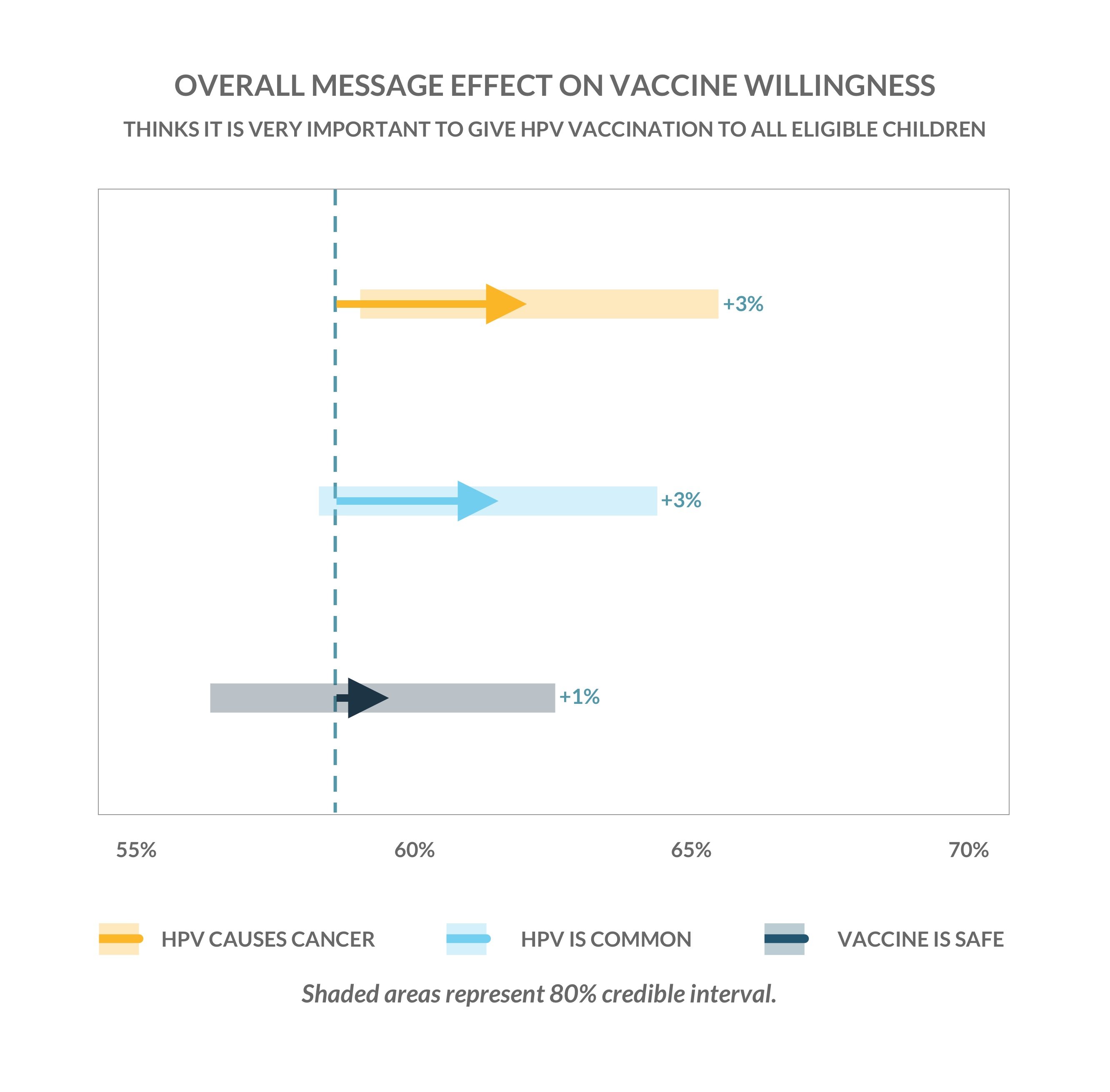
This is an important conclusion: A lot of the prevailing persuasion messaging on vaccination — especially on HPV — is that it’s “safe.” However, a large volume of psychological research (which we won’t dig into here) shows why this is a problem: Defensive messages often cause people to grow further entrenched in their original opinion. We believe that to be the case here.
We recommend that Pro-HPV vaccination campaigns, both in public and in the doctor’s office, should emphasize the consequences — not the safety — of the vaccine.
But let’s dig in a little more about what else is going on here. Contrary to popular opinion, our research reveals that non-vaccinator parents actually know more about HPV than vaccinator parents.
For example, non-vaccinator parents are 11% more likely to know that men can also get HPV. Non-vaccinator parents are also much more likely to know that HPV does not protect against all cancers.
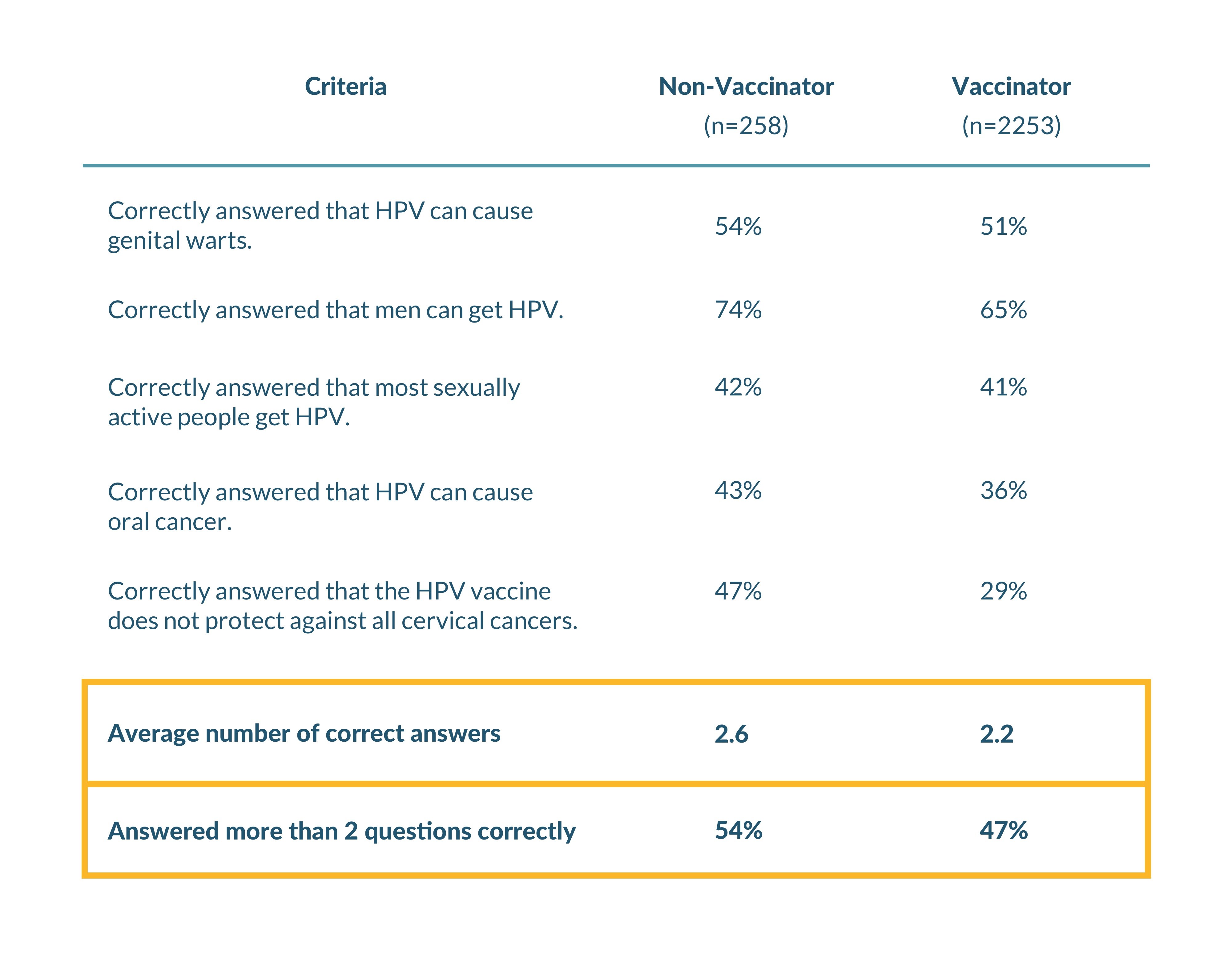
The recommendations from this data aren’t as clear. Our hypothesis is that messaging to non-vaccinators should emphasize the cancers that it can protect against (the positive frame), even though it can’t protect against all cancers.
What’s more, vaccinator parents and non-vaccinator parents get their messages in different places. Vaccinators rely on their doctors, and non-vaccinator parents rely on the media.
While the cause-and-effect relationship here isn’t clear, we can safely assume that vaccinator parents trust their doctors while non-vaccinator parents trust their doctors less and the media more.
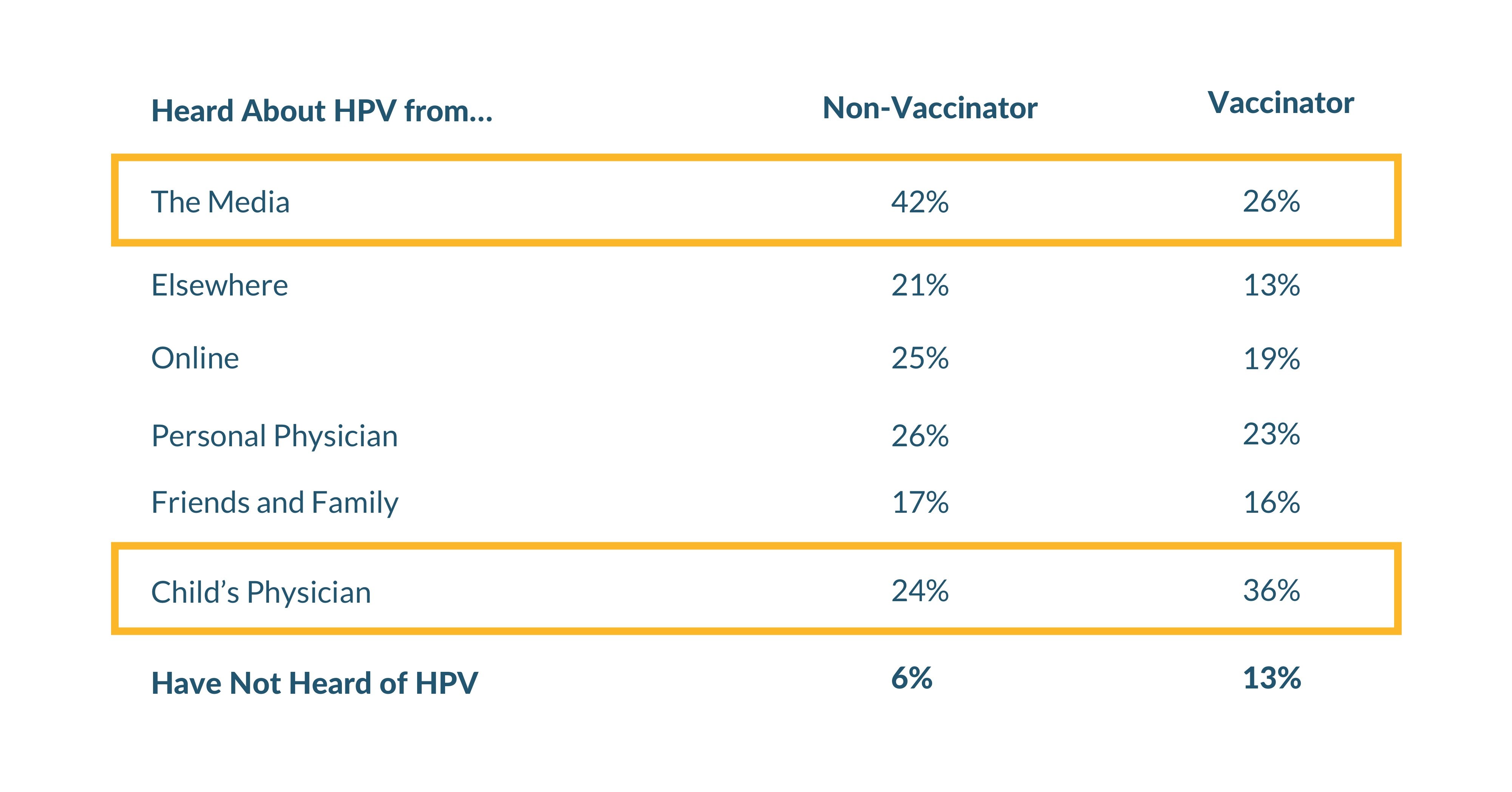
This is unnerving, and it shows the upending of a lot of social norms that we’ve seen in the past 10 years: Increasingly, many people don’t trust experts as much for major decisions—they go to the media instead.
In Summary: What do we do?
We have a few hard recommendations based on our findings:
First, emphasize the consequences of HPV over the safety of the vaccine.
Second, vaccinator campaigns that communicate this message shouldn’t just do so within the walls of the doctor’s office—they should partner with media outlets to do so, as well.
Third, we’ll still need to educate vaccinators on the harms of the disease. Even though we know they’re already inclined to vaccinate, we can’t just rely on them to trust their doctors and the vaccine.
Finally, medical professionals should continue to use these types of simulated online experiments to assess the types of messaging that we can use to convince parents to vaccinate their kids. While this study focused on HPV specifically, we think the same message testing approach can be used across vaccination and treatment communications more broadly.
Have questions or thoughts about this study? We’d love to talk. Candidly, we do provide this type of research and message testing as a service and a technology, so please reach out if you’re interested in hearing about how we can help you.
Thanks –
1Our Methodology
Our message testing methodology is similar to what you might find in a drug trial — in this case, we assigned 2,491 parents into four randomly selected, equally-sized groups in an online panel. Then, three groups received a different pro-vaccination message, and one group received a control message. Afterward, we measured the effect of each message vs. the control group. Additionally, we measured a standard set of survey responses among everyone.